Table of Contents
Key Takeaways
- mRNA vaccines continue to show promise in treating various diseases beyond COVID-19.
- Recent trials have demonstrated enhanced efficacy and safety profiles.
- Policy shifts may influence the future landscape of mRNA vaccine development.
Introduction
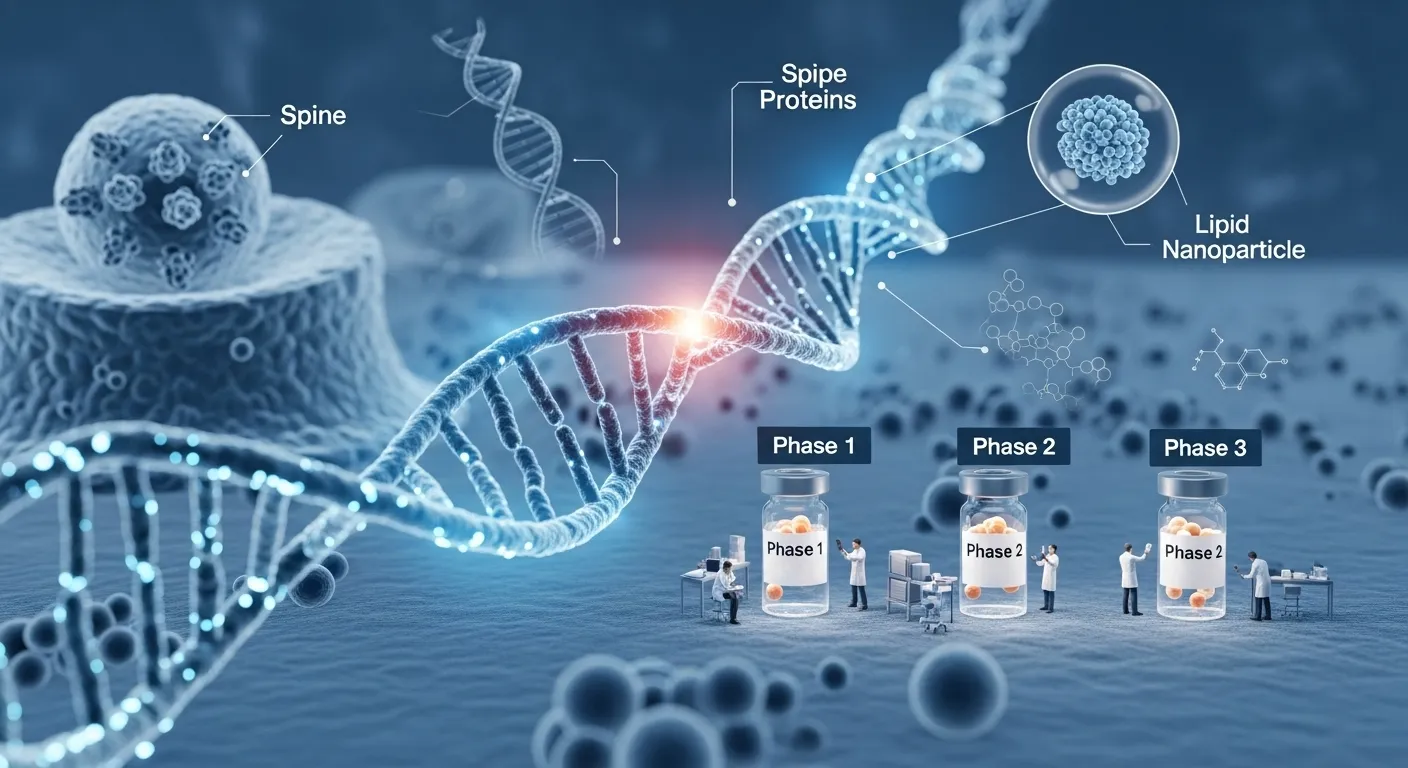
Messenger RNA (mRNA) vaccines continue to transform the landscape of medical research and treatment. Initially popularized by their success against COVID-19, mRNA platforms have quickly expanded to address other pressing health concerns. New clinical data and ongoing research point to even broader applications, increased effectiveness, and the possibility of addressing complex diseases. In fact, some of the most exciting advancements are emerging from clinical trials for triple negative breast cancer, which highlight how mRNA vaccines might offer solutions for diseases that have historically lacked effective treatments.
As scientists refine vaccine formulations and address public health needs, the world is witnessing a new era in immunology—one marked by both scientific triumph and intense policy debate. Amidst these clinical breakthroughs, it’s crucial to consider the influence of regulatory decisions and funding shifts while evaluating how mRNA technology is being harnessed for diseases ranging from seasonal influenza to various forms of cancer.
Moderna’s Experimental Flu Vaccine Shows Enhanced Efficacy
One of the most closely watched mRNA clinical trials involves Moderna’s experimental influenza vaccine (mRNA-1010). In a pivotal study with over 40,000 adult participants aged 50 and older, this vaccine demonstrated a 26.6% higher efficacy compared with a licensed flu vaccine from GlaxoSmithKline (GSK). Importantly, for those aged 65 and older—a population highly vulnerable to flu—Moderna’s mRNA-1010 showed a 27.4% increase in effectiveness. The strong results suggest enhanced immune targeting and better strain matching, raising hopes for improved responses during severe flu seasons and potential pandemics. Moderna is targeting formal regulatory approval and advancing a combined flu-COVID-19 shot, awaiting further efficacy data before a submission. More details can be found via Reuters.
Should the vaccine reach market approval, it could help modernize annual flu vaccination strategies, offering significant public health benefits and potentially curbing the impact of unpredictable flu seasons. Enhanced flexibility in manufacturing and updating mRNA-based shots—thanks to rapid design and synthesis—further boosts optimism among experts. Mainstream health outlets such as Moderna’s official press release have noted that mRNA technologies may soon become the new standard in flu prevention.
FDA Approves Moderna’s Lower-Dose COVID-19 Vaccine
The U.S. Food and Drug Administration (FDA) has approved Moderna’s mNexspike vaccine, a reformulated, lower-dose COVID-19 shot—containing only a fifth of the amount used in Spikevax, its predecessor—aimed at adults aged 65 and older, and those aged 12-64 with at least one high-risk medical condition. The approval follows evidence from a study involving 11,400 participants, which found the new formulation safe and at least as effective, if not superior, in certain respects. Importantly, the FDA mirrored limitations already seen with a Novavax vaccine, highlighting a focus on precision targeting for those with elevated risk profiles.
This decision marks a notable policy change. At the same time, the original Moderna vaccine remains available for all individuals six months and older; the new lower-dose shot is restricted to older adults or at-risk groups. According to Reuters, this reflects a broader regulatory recalibration in response to ongoing epidemiological trends, emerging variant patterns, and the maturing safety dataset for mRNA platforms.
Policy Shifts Impact mRNA Vaccine Development
In August 2025, the U.S. government policy took a turn with the Department of Health and Human Services (HHS) announcing it will wind down many mRNA vaccine development initiatives under its Biomedical Advanced Research and Development Authority (BARDA). This affects 22 projects with an aggregate funding of nearly $500 million. The announcement by HHS Secretary Robert F. Kennedy Jr. comes amid public discourse over the real-world efficacy of mRNA vaccines for respiratory illnesses like COVID-19 and influenza. Despite broad scientific support for mRNA technology, Kennedy cited concerns about “breakthrough” infections and viral mutation, advocating that funding be redirected to vaccine platforms with greater historical resilience and longer-term data.
These policy moves are expected to reshape the research ecosystem for mRNA technology in the U.S. and may influence global investment and collaboration trends. Industry leaders and scientists warn that reduced federal backing could slow progress at precisely the moment when mRNA science is diversifying into new disease areas. The Associated Press provides additional context, detailing both the scientific debate and potential public health implications of these policy decisions. Curious to know more? Read about What Happens When You Stop Taking Sermorelin? | Expert Guide 2025.
Johns Hopkins Explores mRNA for Diverse Treatments
While federal priorities may shift, scientific innovation in mRNA medicine is flourishing in leading university labs. At Johns Hopkins Medicine, researchers leverage mRNA platforms to develop novel therapies for cancer, genetic disorders, and autoimmune diseases. By programming cells to manufacture therapeutic proteins internally, mRNA approaches allow for highly personalized—and potentially transformative—treatment strategies.
Investigators are especially optimistic about mRNA’s role in correcting rare genetic diseases, modulating autoimmune responses, and targeting tumors resistant to conventional therapies. These efforts, detailed in the latest Associated Press coverage, reflect the technology’s vast versatility and the dedication of academic centers to push boundaries even as funding landscapes evolve.
Advancements in Personalized mRNA Cancer Vaccines
Perhaps the most forward-looking application of mRNA technology lies in personalized cancer vaccines. In this approach, vaccines are tailored to target the unique mutations found in a patient’s tumor. Clinical trials are currently underway for a wide range of cancers—including melanoma, pancreatic, and head and neck malignancies—and early results are promising. The British National Health Service’s Cancer Vaccine Launch Pad, for instance, is pioneering collaboration in this area, facilitating trials for bespoke mRNA cancer vaccines across multiple cancer types and patient populations.
Significant attention is being paid to triple-negative breast cancer, an especially aggressive and treatment-resistant form, as researchers hope that mRNA vaccination strategies might offer new hope where few options exist. This highlights the growing importance of ongoing and upcoming clinical trials for triple-negative breast cancer in shaping the future of oncology. For broader insights, Reuters explores how mRNA-based therapies could soon be the backbone of personalized cancer care.
Conclusion
mRNA vaccines are ushering in a new era of precision medicine—offering rapid-response tools against emerging infections and forging inroads into complex chronic diseases like cancer and autoimmune disorders. Ongoing trials in areas like triple-negative breast cancer reflect both the promise and the evolving challenges of this technology. Despite inevitable policy debates and funding uncertainties, the scientific momentum and commitment to innovation remain strong. For patients and healthcare systems worldwide, the expanding scope of mRNA vaccines heralds a future of more effective, accessible, and personalized therapies.